Abstract

Climate change represents a significant and escalating threat to global public health. Rising temperatures, altered precipitation patterns, sea-level rise, and the increasing frequency of extreme weather events have direct and indirect effects on human health. These impacts range from heat-related morbidity and mortality to the spread of infectious diseases, food and water insecurity, and adverse mental health outcomes. This article reviews the major pathways through which climate change affects health, identifies vulnerable populations, and discusses priority strategies for mitigation and adaptation within health systems.
Keywords
Climate change; public health; heat stress; infectious diseases; food security; health systems resilience
1. Introduction
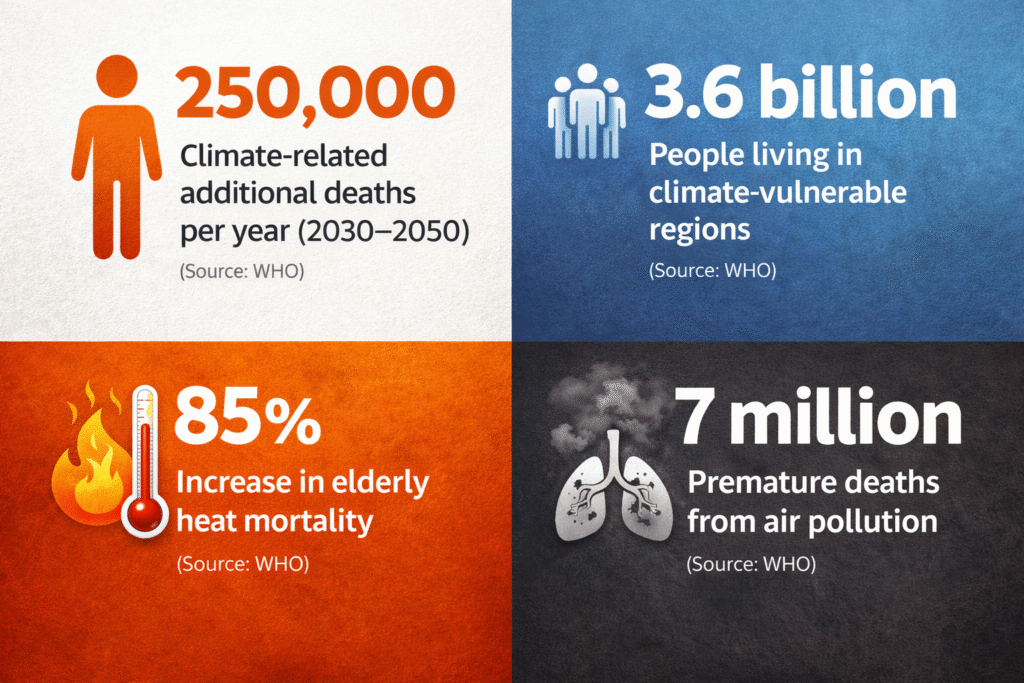
Climate change is no longer solely an environmental or economic issue; it is a critical determinant of population health. Scientific consensus indicates that anthropogenic greenhouse-gas emissions are driving global warming, with measurable consequences for disease patterns, mortality, and health system performance. The World Health Organization has identified climate change as one of the greatest health threats of the 21st century, particularly for low- and middle-income countries with limited adaptive capacity.
2. Direct Health Impacts of Climate Change
2.1 Heat-related morbidity and mortality
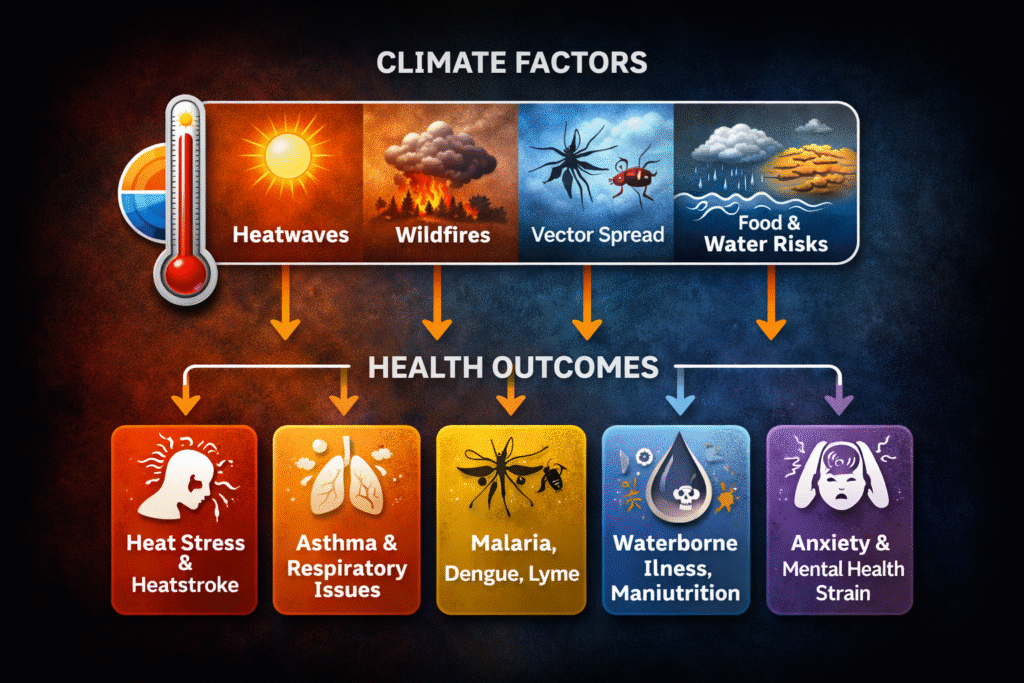
Increasing global temperatures and more frequent heatwaves contribute to heat exhaustion, heatstroke, dehydration, renal dysfunction, and cardiovascular events. Urban populations are especially vulnerable due to the urban heat island effect, inadequate housing, and limited access to cooling.
2.2 Extreme weather events
Climate change intensifies floods, storms, droughts, and wildfires. These events result in immediate injuries and fatalities, disrupt healthcare services, and increase long-term disability and disease burden.
2.3 Air quality deterioration
Higher temperatures exacerbate ground-level ozone formation and increase exposure to particulate matter from wildfires, contributing to respiratory and cardiovascular diseases, including asthma and chronic obstructive pulmonary disease.
3. Indirect Health Impacts
3.1 Infectious diseases
Changes in temperature and rainfall patterns influence the distribution and survival of disease vectors. Vector-borne diseases such as malaria, dengue, and chikungunya are expanding into new geographic areas, increasing exposure among previously unaffected populations.
3.2 Food security and nutrition
Climate-related disruptions to agriculture—through droughts, floods, and heat stress—reduce crop yields and livestock productivity. This increases the risk of undernutrition, micronutrient deficiencies, and food price volatility, with disproportionate effects on children and pregnant women.
3.3 Water-borne diseases
Flooding and water scarcity compromise water quality and sanitation infrastructure, elevating the incidence of diarrheal diseases, including cholera and other enteric infections.
3.4 Mental health outcomes
Climate-related disasters and displacement are associated with anxiety, depression, post-traumatic stress disorder, and other mental health conditions. Chronic climate stressors, such as livelihood loss, further exacerbate psychosocial vulnerability.
4. Vulnerable Populations
The health impacts of climate change are unevenly distributed. Populations at greatest risk include infants and children, older adults, individuals with chronic diseases, outdoor workers, and communities with limited access to healthcare and social protection systems.
5. Public Health Responses
5.1 Mitigation strategies
Reducing greenhouse-gas emissions through clean energy transitions, sustainable transport, and improved urban planning yields substantial co-benefits for health, particularly through improved air quality.
5.2 Adaptation and health system resilience
Health systems must integrate climate risk into planning and service delivery. Priority actions include heat-health action plans, early warning systems for extreme weather, climate-resilient health infrastructure, and strengthened disease surveillance.
5.3 Policy and intersectoral action
Effective responses require coordination across sectors, including environment, energy, agriculture, and urban development, to address the social and environmental determinants of health.
6. Conclusion
Climate change poses a multifaceted and growing threat to human health, with both immediate and long-term consequences. Addressing these challenges requires urgent mitigation to limit future warming, alongside robust adaptation strategies to protect vulnerable populations and strengthen health systems. Recognizing climate change as a core public health issue is essential for safeguarding global health now and in the future.